BACKGROUND: The following content was shared with staff at Michigan Health & Human Services on September 21, 2015. This content was originally presented using Microsoft PowerPoint and some standard details normal in a research paper were omitted due to time and space considerations. (Ex: Attrition was not discussed, links to existing research, etc.)
You may print out a standard (8-1/2″ x 11″) version (8 pages) for ease of readability here: Preemie Growth Project Feasibility Study
Preemie Growth Project Feasibility Study
Ida M Briggs, Michael J Sheehan RHIT
Study Design
This was a feasibility study using a de-identified aggregate limited data set: no IRB review required.
Recruitment began June 11, 2012 and continued through December 31, 2012. Enrollment was open to a heterogeneous group of children from birth through 12 years old displaying mobility issues (including Cerebral Palsy), neuromuscular issues, growth retardation (including failure-to-thrive), cognitive/communication or other developmental delays, or sensory processing issues.
A total of 271 children from 35 states/three provinces and six countries were accepted into the Project. (Two children later formally withdrew.) Of the remaining 269 children, 192 (71.4%) verified they had begun supplementing and were instructed in the reporting process. Data was obtained through a combination of online parent reporting and one-on-one interviews.
Of the 192 children who started supplementation, 160 (83.3%) submitted at least one formal report. Of those 160 children, 134 (83.8%) submitted more than one formal report with an average observation period of 118 days.
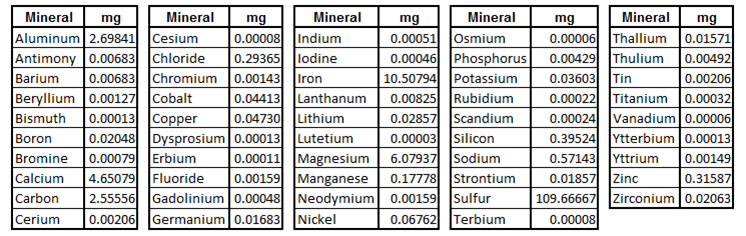
Study protocol: 15 ml of PDCM 72+ once daily (contents per Laboratory Assay)
All contents well within safe levels for Recommended Daily Allowance (RDA), Adequate Intake (AI) or Tolerable Upper Intake Level (UL) (mg/day) per data from the Food and Nutrition Board, Institute of Medicine, National Academies for both infants and adults (spreadsheet available)
Eight categories were tracked
Primary: Muscle tone/strength, Weight/height, Cognition, Communication
Secondary: Bowel function, Appetite, Energy/stamina, Sensory processing
For each of these categories, the parents reported there was either observed change or no change, and then described the change as being positive or negative. For purposes of this project, positive change was considered improvement.
Study Results
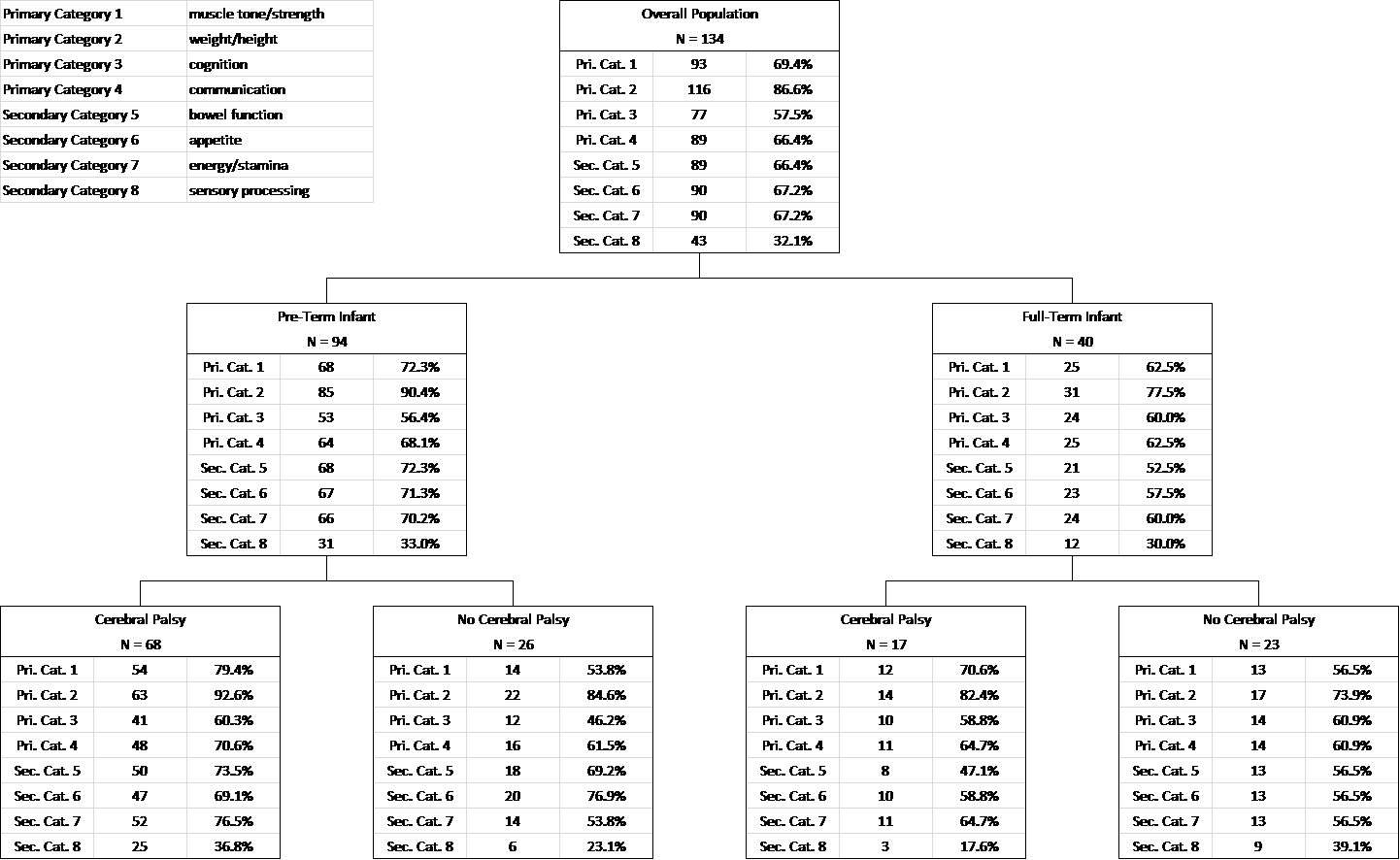
View 1: Preemie vs Full-Term
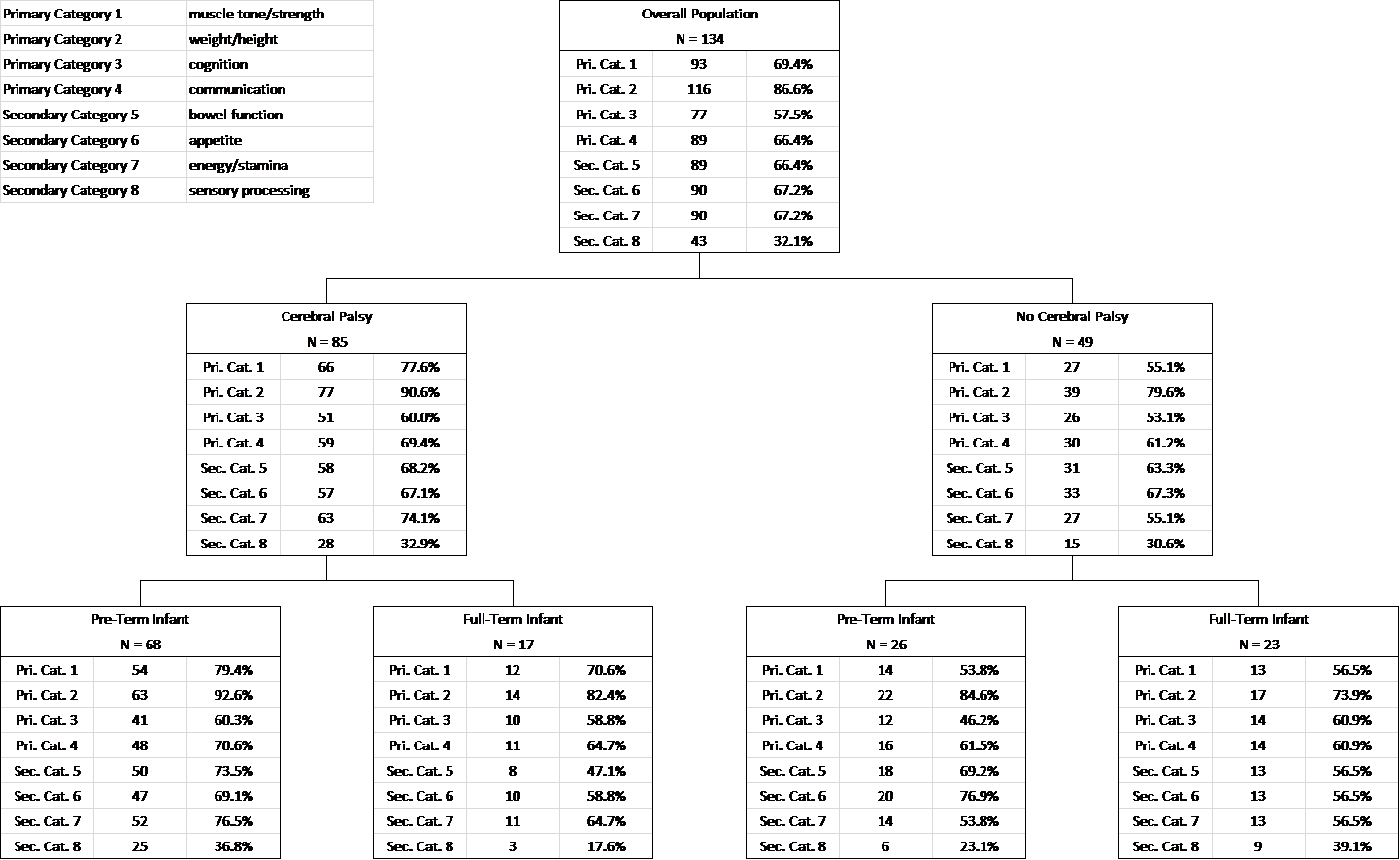
View 2: Cerebral Palsy vs Other
Primary and Secondary Category Analysis
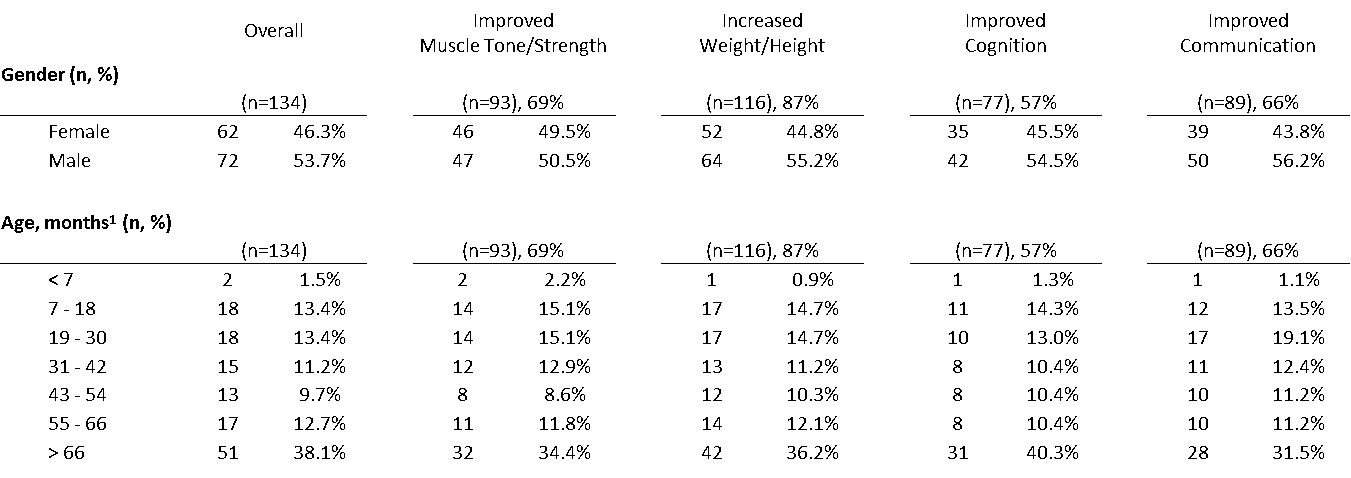
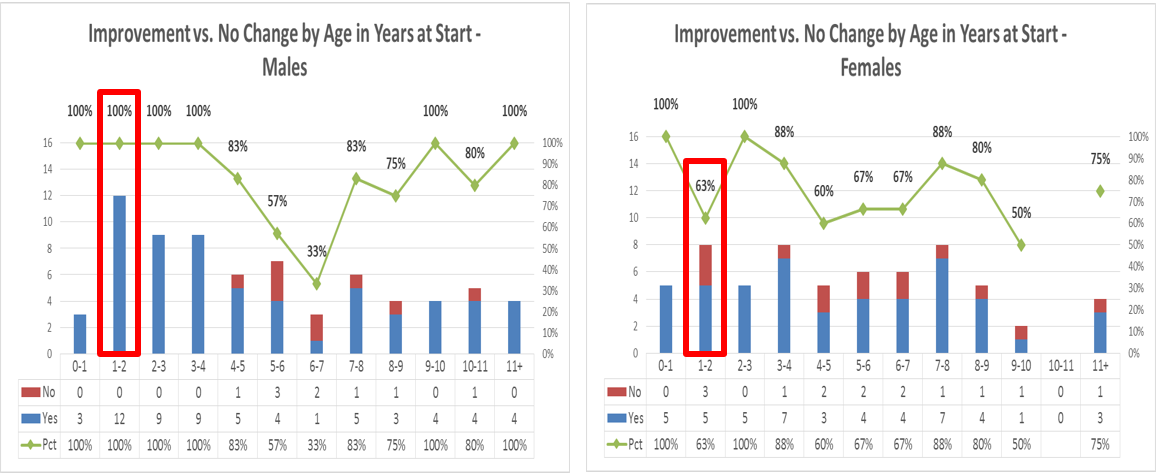
Frequency by Gender & Age, overall and improved subsets
Frequency by Gestational Age & Birth Weight, overall and improved subsets
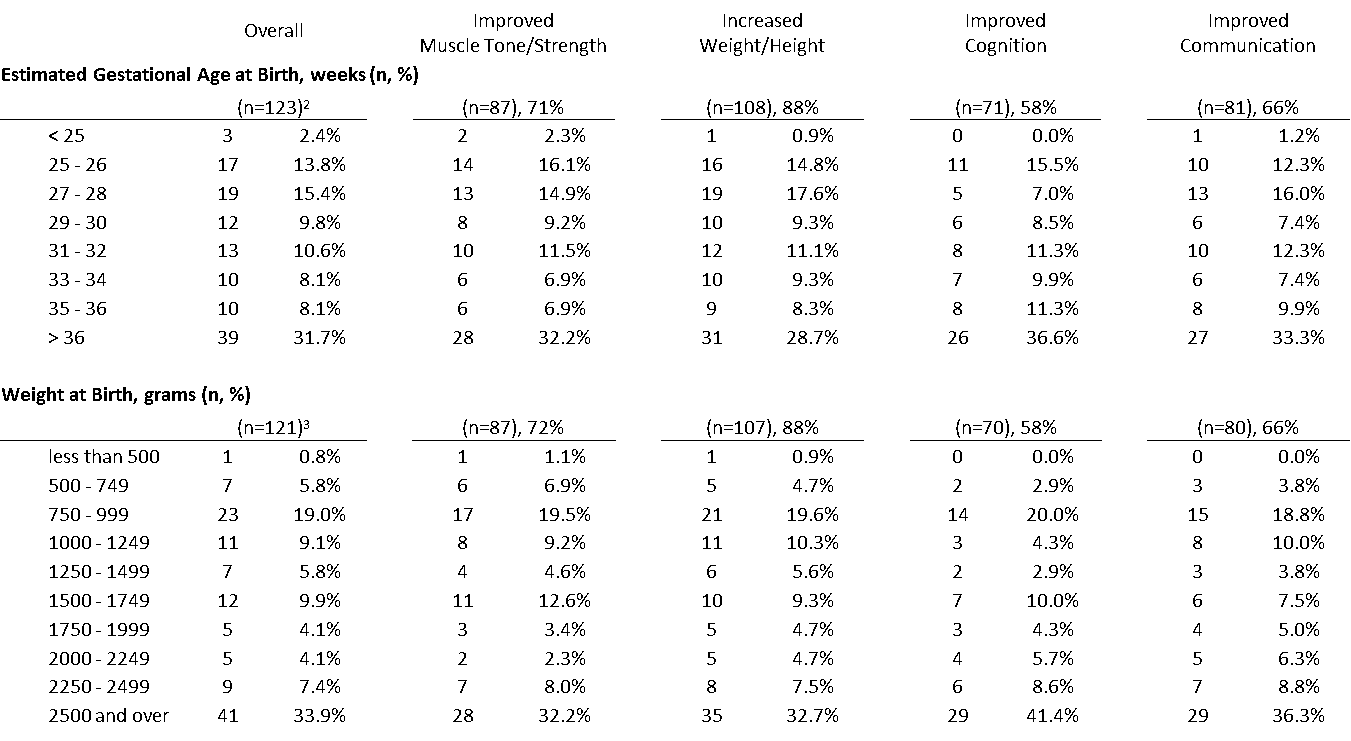
Response to protocol, by Age (Improvement in four or more categories)
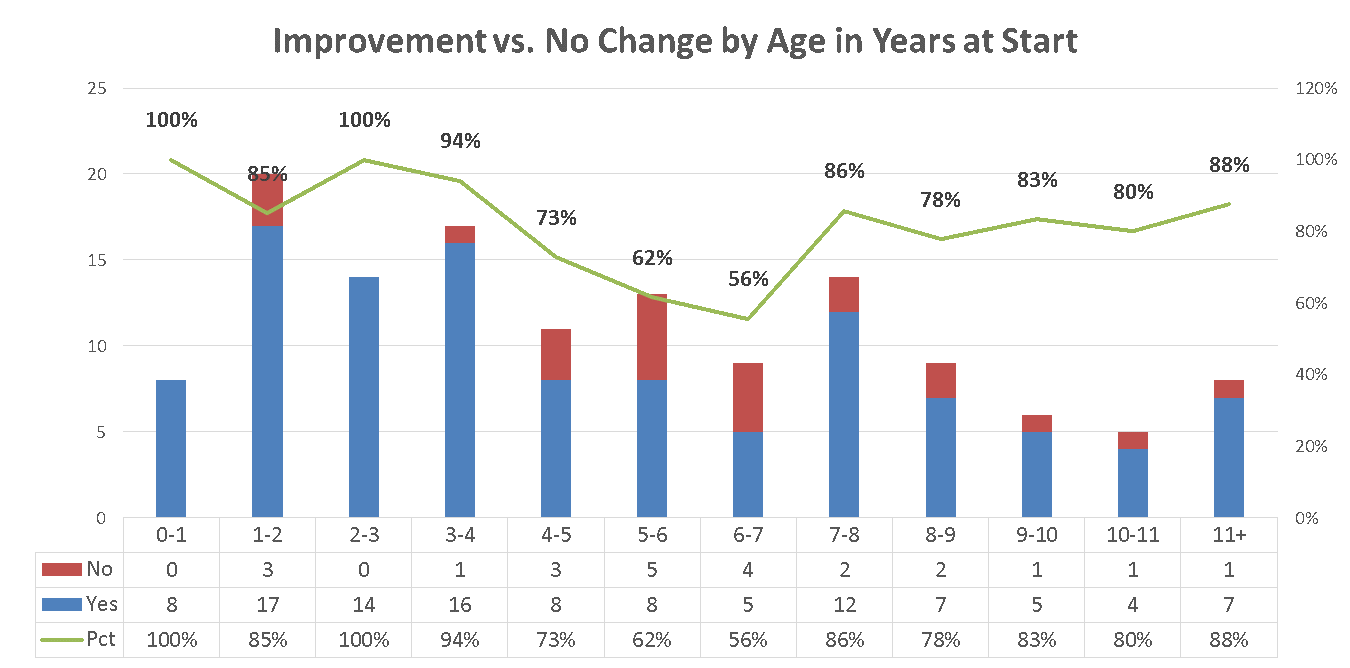
Response to protocol, by Gender and Age (Improvement in four or more categories)
Of particular interest was the slightly higher response rate for males in the 1 to 2 year age range – this runs contrary to known gender disparities in childhood growth and development.
Study Outcomes
134 children were recruited. There were no statistical differences in demographic or baseline characteristics.
During the observation, 93 children (69%) experienced improvement in muscle tone and strength. 116 children (87%) experienced improvement in weight and/or height. 77 children (58%) experienced improvement in cognition. 89 children (66%) experienced improvement in communication.
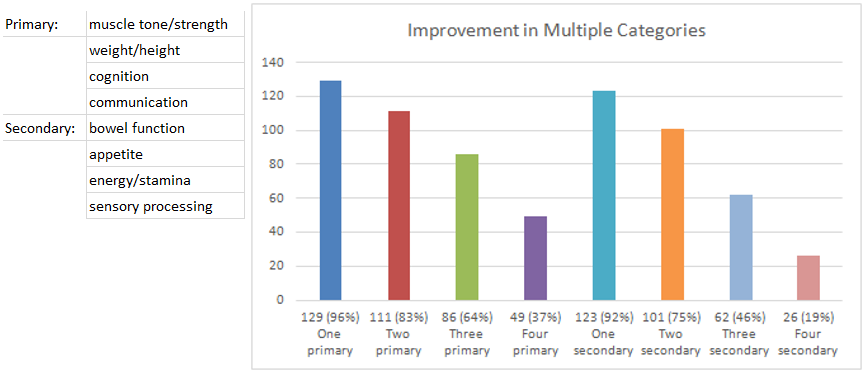
129 children (96%) experienced improvement in at least one primary category. 111 children (83%) experienced improvement in two primary categories. 86 children (64%) experienced improvement in three primary categories. 49 children (37%) experienced improvement in all four primary categories.
Improvement in secondary categories included bowel function (n=89, 66%), appetite (n=90, 67%), energy and stamina (n=90, 67%) and sensory processing (n=43, 32%).
Overall, 111 children (83%) experienced improvement in four or more defined categories.
31 (23%) of the cohort identified as “micro-preemies” (weighing less than 1000 grams at birth); 28 of those (90%) reported improvement in four or more defined categories.
Observed Patterns of Improvement
Infants responded faster, in some cases in as little as 24-72 hours. Young children appeared to respond faster than older children.
The first change was usually in bowel function, occurring within the first ten days. This appeared to correspond with an increase in intestinal strength and decrease in constipation issues.
Around 14 days there was an increase in appetite. Again, in infants the change was faster, while older children commonly reported it between days 14 and 21.
Changes in weight and/or height, muscle tone and/or strength, cognition, communication, energy and/or stamina and sensory processing were usually being reported within six weeks.
Despite a high percentage of chronic failure-to-thrive issues in this population, weight and height gains were similar to the patterns seen in non-failure-to-thrive children.
Head circumference changes (if reported) were usually noted within 90 to 120 days.
Muscle tone and/or strength changes typically were reported in the following order:
- Increased trunk and neck strength (core muscles)
- Increased strength in extremities
- Hyperspastic muscles “relaxed” at first, then those “weak” muscles got stronger
Sensory processing issues (especially in children with a history of ear infections and/or heavy antibiotic use) were usually controlled within 16 weeks.
It was reported several medically fragile children experienced a significant drop in unplanned hospitalizations.
Study Discussion
What does this mean for children diagnosed with Cerebral Palsy?
By definition, Cerebral Palsy (CP) is a group of non-progressive permanent motor disorders that appear in early childhood. Since CP is permanent, any child whose movement disorder improved when their micronutrient deficiency was corrected may never have had CP in the first place – they may have been misdiagnosed.
The ability of increased micronutrient intake to correct deficiency may also explain the small percentage of children under age 4 whose CP symptoms spontaneously resolve – they may be eating a healthier diet that is particularly rich in micronutrients. Self-correction of a nutritional deficit is a reasonable explanation for previously unexplained rare improvement.
Is there any precedent for this “misdiagnosed Cerebral Palsy” theory?
In the 1990s pediatric research established new testing protocols to identify the group of conditions called “inborn errors of metabolism”. Before these tests were developed, patients with movement disorder symptoms would have been placed under the umbrella diagnosis of Cerebral Palsy, and subsequent treatment would have progressed without addressing the underlying disorder. Re-defining these cases as caused by inborn errors of metabolism led to developing specific treatment protocols with substantial improvements in outcomes.
Identifying children whose growth issues are caused by correctable trace mineral deficiency could prevent a potentially common misdiagnosis of Cerebral Palsy.
A Few Words of Caution
Just like when introducing new foods (strawberries, peanuts, etc.) parents should monitor for any sensitivity reactions.
- Absence seizures were experienced by two children, which stopped when they ceased taking the supplement.
- Multiple parents reported minor rashes (red spots on trunk) which went away without intervention within a few days.
- In infants the improvement in bowel function and increased appetite also came with an increase in dirty diapers and a greater risk of diaper rash.
Multiple parents also reported mood swings which they later determined were associated with being hungry; parents were encouraged to offer healthy, nutritious snacks even if they were previously unused to having hungry children.
This may not be an appropriate intervention for children with a history of seizures; parents whose children have these conditions need to be especially vigilant as changes in weight/increased growth may impact the efficacy of medications.
Long-term use of laxative solutions containing Polyethylene Glycol 3350 (such as Miralax) is known to hinder absorption of micronutrients, and therefore children in a deficiency state should not use it regularly.
Study Conclusions
- Micronutrient deficiency results in growth retardation in human beings as well as animals, which includes
- poor growth and appetite
- impaired immune responses
- weak muscles
- developmental delays
- and “general ill-thrift”
- It presents in different ways during the life cycle
- At birth, as low birth weight or premature babies
- In infancy, as failure-to-thrive and developmental delays
- In childhood, the weak muscles (especially core) are diagnosed as cerebral palsy
- Deficiencies also present as other neuromuscular issues, including sensory processing issues
- Two key indicators of probable deficiency are low birth weight and weak core strength.
- Early oral correction reduces these symptoms, which should result in lowered rates of infant mortality and morbidity, and healthier childhood populations